doctors' treatment
arthritis
Arthritis is a form of joint disorder that involves inflammation of one or more joints. There are over 100 different forms of arthritis.[3][4] The most common form, osteoarthritis (degenerative joint disease), is a result of trauma to the joint, infection of the joint, or age. Other arthritis forms are rheumatoid arthritis, psoriatic arthritis, and related autoimmune diseases. Septic arthritis is caused by joint infection.
Signs and symptoms
Pain, which can vary in severity, is a common symptom in virtually all types of arthritis.,Other symptoms include swelling, joint stiffness and aching around the joint(s). Arthritic disorders like lupus and rheumatoid arthritis can affect other organs in the body, leading to a variety of symptoms. Symptoms may include:

- Inability to use the hand or walk
- Stiffness, which may be worse in the morning, or after use
- Malaise and fatigue
- Weight loss
- Poor sleep
- Muscle aches and pains
- Tenderness
- Difficulty moving the joint
It is common in advanced arthritis for significant secondary changes to occur. For example, arthritic symptoms might make it difficult for a person to move around and/or exercise, which can lead to secondary effects, such as:
- Muscle weakness
- Loss of flexibility
- Decreased aerobic fitness
These changes, in addition to the primary symptoms, can have a huge impact on quality of life.
Knee replacement
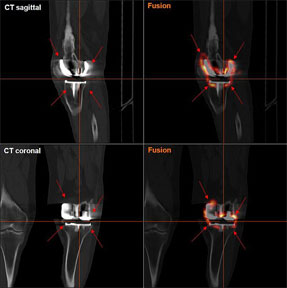
Knee replacement, or knee arthroplasty, is a surgical procedure to replace the weight-bearing surfaces of the knee joint to relieve pain and disability. It is most commonly performed for osteoarthritis,and also for other knee diseases such as rheumatoid arthritis and psoriatic arthritis. In patients with severe deformity from advanced rheumatoid arthritis, trauma, or long-standing osteoarthritis, the surgery may be more complicated and carry higher risk. Osteoporosis does not typically cause knee pain, deformity, or inflammation and is not a reason to perform knee replacement.
Other major causes of debilitating pain include meniscus tears, cartilage defects, and ligament tears. Debilitating pain from osteoarthritis is much more common in the elderly.
Knee replacement surgery can be performed as a partial or a total knee replacement. In general, the surgery consists of replacing the diseased or damaged joint surfaces of the knee with metal and plastic components shaped to allow continued motion of the knee.
The operation typically involves substantial postoperative pain, and includes vigorous physical rehabilitation. The recovery period may be 6 weeks or longer and may involve the use of mobility aids (e.g. walking frames, canes, crutches) to enable the patient's return to preoperative mobility.
Risks
- Deep vein thrombosis
According to the American Academy of Orthopedic Surgeons (AAOS), deep vein thrombosis in the leg is "the most common complication of knee replacement surgery... prevention... may include periodic elevation of patient's legs, lower leg exercises to increase circulation, support stockings and medication to thin your blood
- Fractures
Periprosthetic fractures are becoming more frequent with the aging patient population and can occur intraoperatively or postoperatively.
- Loss of Motion
The knee at times may not recover its normal range of motion (0–135 degrees usually) after total knee replacement. Much of this is dependent on pre-operative function. Most patients can achieve 0–110 degrees, but stiffness of the joint can occur. In some situations, manipulation of the knee under anesthetic is used to reduce post operative stiffness. There are also many implants from manufacturers that are designed to be "high-flex" knees, offering a greater range of motion.
- Instability
In some patients, the kneecap is unrevertable post-surgery and dislocates to the outer side of the knee. This is painful and usually needs to be treated by surgery to realign the kneecap. However this is quite rare.
In the past, there was a considerable risk of the implant components loosening over time as a result of wear. As medical technology has improved however, this risk has fallen considerably. Knee replacement implants can now last up to 20 years.
Pelvis and Acetabulum
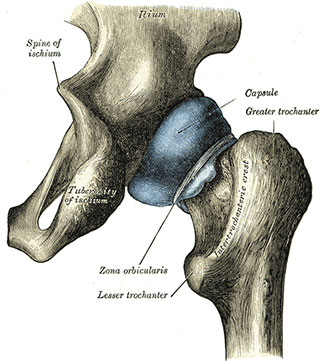
The acetabulum is a concave surface of the pelvis. The head of the femur meets with the pelvis at the acetabulum, forming the hip joint.
Pelvic bone is a very complex structure. This is bone is felt inside your waist region. It protects vital internal structures and has extensive blood supply. Acetabulum is a cup or a socket like structure forming a part of your hip joint. This participates in the ball and socket mechanism of the joint. Acetabulum is a part of your pelvic bone. Acetabulum carries your body weight across your lower limbs and hence it is important to fix any fractures of this bone accurately to prevent joint pain and arthritis in the future.
Pelvic-acetabular fractures are one of the most severe orthopaedic injuries. Pelvic fractures are prone for severe internal bleeding and can cause shock and death. Acetabular fractures can lead to long term morbidity like hip pain, arthritis and difficulty in mobilisation. Fixing both of these fractures is a very difficult task mainly because of their complex structure and proximity to vital structures, blood vessels and important nerves going to legs.
To many orthopaedic surgeons, the mere mention of pelvic or acetabular fractures gives rise to images of severe trauma such as a motorcyclist with a badly displaced both-column acetabular fracture, or a patient in hypovolemic shock due to an open-book pelvic fracture or other traumatic injuries.
Orthopaedic surgeons in private practice rarely see injuries of this magnitude, and they quickly, happily, and appropriately refer such patients to orthopaedic trauma surgeons whenever possible.
The intent of this article, therefore, is not to discuss the esoteric details of these complex fractures, but to review the conundrums associated with the more common pelvic and acetabular fractures seen in emergency departments across the country.
A quick word on the more severe injuries, however, is appropriate. Fortunately, patients with significant pelvic trauma are often transported to a trauma center where they can be treated by a well-prepared team of trauma surgeons and staff. Advanced Trauma Life Support protocols aptly describe the methods of evaluation and resuscitation of trauma patients. Because the hemorrhage associated with an open-book pelvic fracture can be considerable and life-threatening, patients with a severe anteroposterior compression (APC) injury with diastasis of the symphysis and sacroiliac joint(s) should be immediately stabilized, using one of several methods to decrease pelvic volume. These methods include pelvic binders, MAST trousers, a C-clamp, or wrapping a sheet around the pelvis.
hip replacement
Hip replacement is a surgical procedure in which the hip joint is replaced by a prosthetic implant. Hip replacement surgery can be performed as a total replacement or a hemi (half) replacement. Such joint replacement orthopaedic surgery is generally conducted to relieve arthritis pain or in some hip fractures. A total hip replacement (total hip arthroplasty) consists of replacing both the acetabulum and the femoral head while hemiarthroplasty generally only replaces the femoral head. Hip replacement is currently the most common orthopaedic operation, though patient satisfaction short- and long-term varies widely.

Risks
- Vein thrombosis
Venous thrombosis such as deep vein thrombosis and pulmonary embolism are relatively common following hip replacement surgery. Standard treatment with anticoagulants is for 7–10 days; however treatment for more than 21 days may be superior.
Some physicians and patients may consider having lower limbs venous ultrasonography to screen for deep vein thrombosis after hip replacement.However, this kind of screening should only be done when indicated because to perform it routinely would be unnecessary health care.
- Dislocation
Dislocation is the most common complication of hip replacement surgery. At surgery the femoral head is taken out of the socket, hip implants are placed and the hip put back into proper position. It takes eight to twelve weeks for the soft tissues injured or cut during surgery to heal. During this period, the hip ball can come out of the socket. The chance of this is diminished if less tissue is cut, if the tissue cut is repaired and if large diameter head balls are used. Surgeons who perform more of the operations each year tend to have fewer patients dislocate. Doing the surgery from an anterior approach seems to lower dislocation rates when small diameter heads are used, but the benefit has not been shown when compared to modern posterior incisions with the use of larger diameter heads. Patients can decrease the risk further by keeping the leg out of certain positions during the first few months after surgery. Use of alcohol by patients during this early period is also associated with an increased rate of dislocation.
- Fracture
Bones with internal fixation devices in situ are at risk of periprosthetic fractures at the end of the implant, an area of relative mechanical stress. Post-operative femoral fractures are graded by the Vancouver classification.
- Osteolysis
Many long-term problems with hip replacements are the result of osteolysis. This is the loss of bone caused by the body's reaction to polyethylene wear debris, fine bits of plastic that come off the cup liner over time. An inflammatory process causes bone resorption that may lead to subsequent loosening of the hip implants and even fractures in the bone around the implants. In an attempt to eliminate the generation of wear particles, ceramic bearing surfaces are being used in the hope that they will have less wear and less osteolysis with better long-term results. Metal cup liners joined with metal heads (metal-on-metal hip arthroplasty) were also developed for similar reasons. In the lab these show excellent wear characteristics and benefit from a different mode of lubrication. At the same time that these two bearing surfaces were being developed, highly cross linked polyethylene plastic liners were also developed. The greater cross linking significantly reduces the amount of plastic wear debris given off over time. The newer ceramic and metal prostheses do not always have the long-term track record of established metal on poly bearings. Ceramic pieces can break leading to catastrophic failure. This occurs in about 2% of the implants placed. They may also cause an audible, high pitched squeaking noise with activity. Metal-on-metal arthroplasty releases metal debris into the body raising concerns about the potential dangers of these accumulating over time. Highly cross linked polyethylene is not as strong as regular polyethylene. These plastic liners can crack or break free of the metal shell that holds them.